It's a New Day in Public Health.
The Florida Department of Health works to protect, promote, and improve the health of all people in Florida through integrated state, county, and community efforts.
Antimicrobial Resistance
What are antibiotics?
Any substance that inhibits the growth and replication of a bacterium or kills it outright can be called an antibiotic. Antibiotics are a type of antimicrobial designed to target bacterial infections within (or on) the body.
When can antibiotics help?
Antibiotics are used to treat bacterial infections. Some are highly specialized and are only effective against certain bacteria. Others, known as broad spectrum antibiotics, attack a wide range of bacteria, including ones that are beneficial to us.
There are two main ways in which antibiotics target bacteria. They either prevent the reproduction of bacteria, or they kill the bacteria, for example by stopping the mechanism responsible for building their cell walls.
| Common Condition |
| Are Antibiotics Needed? | ||||||
|---|---|---|---|---|---|---|---|---|
| Strep throat | Yes | |||||||
| Whooping cough | Yes | |||||||
| Urinary tract infection | Yes | |||||||
| Sinus infection | Maybe | |||||||
| Middle ear infection | Maybe | |||||||
| Bronchitis/chest cold (in otherwise healthy children and adults)* | No* | |||||||
| Common cold/runny nose | No | |||||||
| Sore throat (except strep) | No | |||||||
| Flu | No | |||||||
Why is it important to take antibiotics only when they’re needed?
Antibiotics are important to treat infections and have saved countless lives. However, anytime antibiotics are used, they can cause side effects and contribute to antibiotic resistance, one of the most urgent threats to the public’s health.
What are resistant bacteria?
Each time you take an antibiotic, bacteria are killed. Sometimes, bacteria causing infections are already resistant to prescribed antibiotics. Bacteria may also become resistant during treatment of an infection. Resistant bacteria do not respond to the antibiotics and continue to cause infection. A common misconception is that a person’s body becomes resistant to specific medicines. However, it is the bacteria, not people, that become resistant to the medicines.
Why should I care about antibiotic resistance?
Antibiotic resistance can affect any person, at any stage of life. People receiving health care or those with weakened immune systems are often at higher risk for getting an infection.
Antibiotic resistance jeopardizes advancements in modern health care that we have come to rely on, such as joint replacements, organ transplants, and cancer therapy. These procedures have a significant risk of infection, and patients won’t be able to receive then if effective antibiotics are not available.
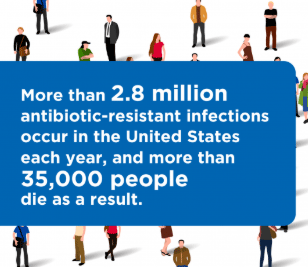
Fighting this threat is a public health priority that requires a collaborative global approach across sectors.
Infections caused by antibiotic-resistant germs are difficult, and sometimes impossible, to treat. In most cases, antibiotic-resistant infections require extended hospital stays, additional follow-up doctor visits, and costly and toxic alternatives.
*Note: This page contains materials in the Portable Document Format (PDF). The free Acrobat Reader may be required to view these files.



Connect with DOH