When the airways react, the lining of the airways become inflamed, the muscles around them tighten, causing a narrowing of the airways, and the cells in the airways might make more mucus than usual. These reactions cause less air flow into the lungs making it harder to breathe.
Approximately 1 in 11 (9.3%) Florida adults and 1 in 14 (7.1%) Florida children currently have asthma. In addition to considerable impacts on quality of life, the economic cost of asthma is sizeable. Direct medical costs (such as hospital admissions, emergency room visits, and the cost of pharmaceuticals) and indirect costs (such as time lost from work, school absenteeism, and premature death) weigh heavily on individuals, the health care system, and schools.
Cause and Triggers
An asthma episode can happen when you are exposed to “asthma triggers” or something to which you are sensitized. Your triggers can be very different from those of someone else with asthma. You may react to just one trigger or you may find that several things act as triggers.
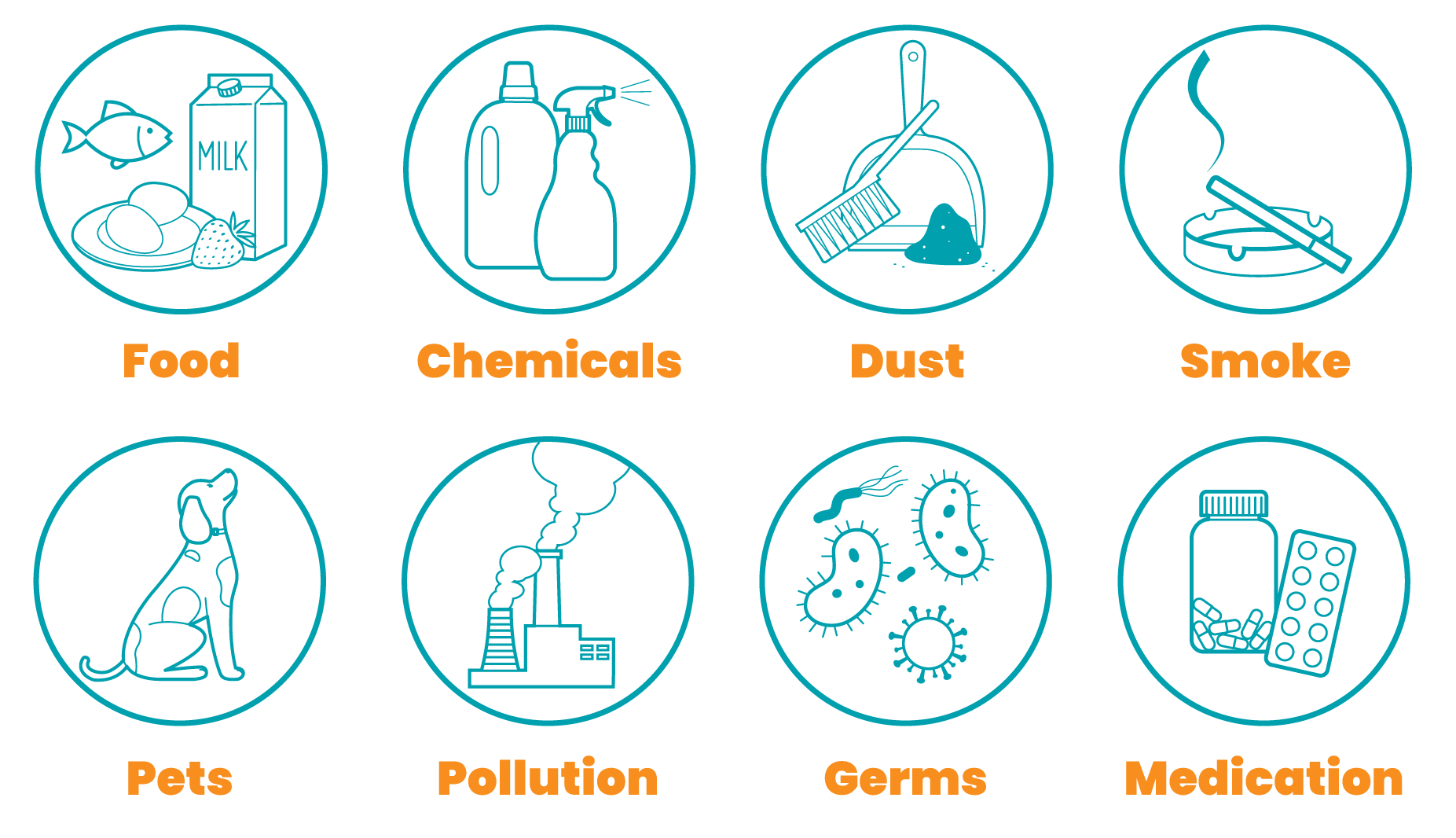
Knowing your triggers and learning how to avoid them are simple actions you can take to control your asthma. Although there is no cure for asthma, most people can control asthma so that they have fewer symptoms and can live healthy, active lives.
Common Triggers
Allergens
- Indoor mold
- Pollens from trees, grasses, and plants
- Animal dander and saliva
- Dust mites
- Cockroaches
Irritants
- Tobacco smoke
- Wood burning smoke
- Perfumes and sprays
- Household chemicals
- Strong odors
- Air pollution
Other
- Flu and cold virus
- Sulfites (used as a preservative in foods)
- Cold air or extreme weather changes
- ExerciseExtreme emotion such as crying or laughing
For more information about trigger identification and ways to reduce your exposure, visit the Environmental Protection Agency.
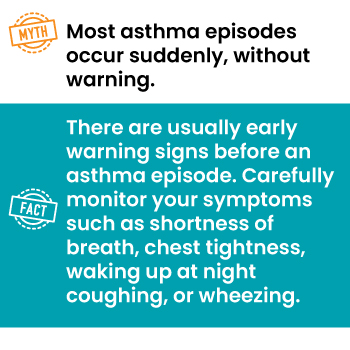
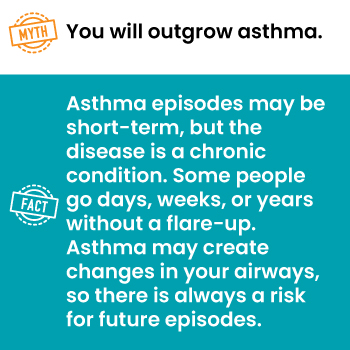
Symptoms
Most people with asthma go for periods of time without any symptoms, then have a sudden asthma flare or episode. Some people have chronic shortness of breath that gets worse during a flare. Asthma flares can last minutes to days and can become dangerous if airflow to the lungs becomes severely restricted.
Signs and symptoms of asthma vary from person to person. They may also vary for a person depending on which trigger they have been exposed to. Primary symptoms include:
- Shortness of breath
- Wheezing
- Chest tightness
- Nighttime coughing (dry or with sputum)
Emergency care should be sought if any of the following are experienced:
- In infants, head bobbing
- Extreme difficulty breathing or stopping breathing
- Bluish color to the lips, fingernails, and face, called cyanosis
- Struggling to talk or stay awake
- Chest retractions (having to strain your chest muscles to breathe)
Diagnosis
Your health care provider will diagnose asthma based on your medical and family history, physical exam, and test results. They will also determine the severity of your asthma to establish what treatment options are available for you.
Your health care provider may ask you about related health conditions that can interfere with asthma management. These conditions include a nasal allergy, sinus infections, reflux disease, psychological stress, and sleep apnea.
You may also have lung function tests to measure how much air your lungs can hold and how much air you breathe out. Your health care provider may use a spirometer to measure how much air you exhale and how quickly you get air out of your lungs. Other tests may include chest and sinus x-rays, blood tests, or allergy tests.
Managing Asthma
Asthma Medications and Devices
Long-Term Control Medications
Quick-Relief Medications
Prescription Assistance
Asthma Action Plan
If you have asthma, you should have an asthma action plan. The plan is individualized that has daily treatment outlined, including medication and when to take them.
Work with your health care provider to develop an action plan tailored to your asthma management, and updated as needed. People involved in the care should be made aware of the asthma action plan, including school and childcare center workers.
Action Plan Resources
Asthma Myths and Facts
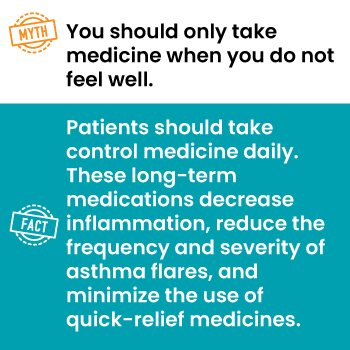
![Myth: There is nothing you can do to make your asthma improve.
Fact: There are different ways to control asthma, such as reducing exposure to triggers, taking[sic] medication as prescribed, and communicating[sic] with your healthcare[sic] provider.](https://www.floridahealth.gov/wp-content/uploads/2024/10/Asthma4.jpg)


About the Florida Asthma Program
Florida Asthma Program
The Florida Asthma Program coordinates statewide efforts to reduce asthma and hospitalization rates, as well as increase the number of people with asthma receiving self-management education.
The program provides comprehensive asthma care by ensuring access to guidelines-based medical management and linking those with poorly controlled asthma to health care services.
National Asthma Control Partner
Florida providing comprehensive care along with other state partners to improve the quality of asthma care, asthma management in schools, and foster policies to help reduce exposure to asthma triggers in outdoor, indoor, and workplace environments.
- Develops, manages, tracks, and analyzes a set of asthma health status indicators that are derived from a variety of sources and accommodate state and local asthma related data needs through the statewide asthma surveillance system.
- Engages community partners to increase community readiness to identify gaps in the delivery of asthma-related programs and services to improve Florida’s existing asthma system of care.
- Promotes and expands quality asthma self-management education and reduce exposure to asthma triggers through a home-visiting environmental assessment.
- Facilitates the Florida Asthma Coalition to address asthma rates in communities, improve quality of life, and reduce costs
- Increases public awareness of the importance of reducing the burden of asthma and the need for supportive policies and environments
Information for Health Care Providers
Since the Guidelines for the Diagnosis and Management of Asthma (EPR-3) was released in 2007, researchers have made substantial progress in understanding asthma diagnosis, management, and treatment.
Based on systematic reviews conducted by the Agency for Healthcare Research and Quality With and input from National Asthma Education Prevention Program (NAEPP) participant organizations, medical experts, and the public, the NHLBI supported the development of the 2020 Focused Updates to the Asthma Management Guidelines: A Report from the National Asthma Education and Prevention Program Coordinating Committee Expert Panel Working Group.
Resources
National Environmental Education Foundation: Partnered with CDC, the National Asthma Control Program and developed guidelines for environmental management of pediatric asthma.
American Lung Association Professional Education: Tracks the coverage and related barriers to asthma guidelines-based care in state Medicaid programs.
Allergy and Asthma Foundation of America: Continuing education for health care professionals who teach and care for patients with asthma. The online course has been approved for 8.75 contact hours by the American Association of Respiratory Care and the American Nurses Credentialing Center’s Commission on Accreditation.
American Academy of Allergy Asthma & Immunology: Offers education on discoveries in allergy and immunology, supporting licensing and certification needs.
Allergy and Asthma Network: Works in partnership with the health care community to provide connections to conferences, meetings, and CME opportunities.
Asthma Management Guidelines for Health Care Professionals: Free training designed to help health care professionals learn and apply guidelines-based asthma care.
Data and Surveillance
Data are compiled to assess the burden of asthma in Florida, and to monitor and evaluate the impact and effectiveness of efforts over time.