Any substance that inhibits the growth and replication of a bacterium or kills it outright can be called an antibiotic. Antibiotics are a type of antimicrobial designed to target bacterial infections within (or on) the body.
Some are highly specialized and are only effective against certain bacteria. Others, known as broad spectrum antibiotics, attack a wide range of bacteria, including ones that are beneficial to us.
There are two main ways in which antibiotics target bacteria. They either prevent the reproduction of bacteria, or they kill the bacteria.
Antibiotic Resistant Bacteria
Each time you take an antibiotic, bacteria are killed. Sometimes, bacteria causing infections are already resistant to prescribed antibiotics. Bacteria may also become resistant during treatment of an infection. Resistant bacteria do not respond to the antibiotics and continue to cause infection. A common misconception is that a person’s body becomes resistant to specific medicines. However, it is the bacteria, not people, that become resistant to the medicines.
Antibiotic resistance can affect any person, at any stage of life. People receiving health care or those with weakened immune systems are often at higher risk for getting an infection.
Antibiotic resistance jeopardizes advancements in modern health care that we have come to rely on, such as joint replacements, organ transplants, and cancer therapy. These procedures have a significant risk of infection, and patients won’t be able to receive then if effective antibiotics are not available.
Fighting this threat is a public health priority that requires a collaborative global approach across sectors.
Infections caused by antibiotic-resistant germs are difficult, and sometimes impossible, to treat. In most cases, antibiotic-resistant infections require extended hospital stays, additional follow-up doctor visits, and costly and toxic alternatives.
Take Antibiotics Only When Needed
Many medical advances are dependent on the ability to fight infections using antibiotics, including joint replacements, organ transplants, cancer therapy and the treatment of chronic diseases like diabetes, asthma, and rheumatoid arthritis.
If antibiotics or antifungals lose their effectiveness, then we lose the ability to treat infections and control these public health threats.
- Talk with your health care provider about the best treatment when you or your family are sick.
- Talk with your veterinarian about the best treatment option when your animal is sick.
- Antibiotics and antifungals save lives, but any time they are used they can cause sides effects and contribute to antimicrobial resistance.
| Condition | Bacteria | Bacteria or Virus | Virus | Antibiotics Needed |
|---|---|---|---|---|
| Strep throat | X | Yes | ||
| Whooping cough | X | Yes | ||
| Urinary tract infection | X | Yes | ||
| Sinus infection | X | Maybe | ||
| Middle ear infection | X | Maybe | ||
| Bronchitis/chest cold (in otherwise healthy children and adults)* | X | No* | ||
| Common cold/runny nose | X | No | ||
| Sore throat (except strep) | X | No | ||
| Flu | X | No |
Information for Health Care Providers
Antibiotic Stewardship
Antibiotic stewardship has several proven benefits that include protecting patients from unintended consequences, improving treatment of infections, and helping combat antibiotic resistance. These data reflect programs in acute care hospital settings.
Core Elements of Antibiotic Stewardship
Gives providers and facilities a set of key principles to guide efforts to improve antibiotic use and, therefore, advance patient safety and improve outcomes.
Antibiotic Stewardship Resources
Florida
- Antimicrobial Stewardship Program Toolkit
- Antibiotic Stewardship Profile
- Core Elements of Antibiotic Stewardship
Hospitals
- Core Elements of Hospital Stewardship
- Program Assessment Tool
- Implementation at Small and Critical Access Hospitals
- Implementation for Hospitals
- Core Elements for Nursing Homes
- Checklist: Core Elements for Nursing Homes
- Implementation for Nursing Homes
Outpatient Facilities
Tracking CRE
Bacteria are constantly finding new ways to avoid the effects of antibiotics. For example, some Enterobacteriaceae can produce enzymes called carbapenemases that break down antibiotics including carbapenems, making the drugs ineffective. Carbapenem antibiotics are typically reserved to treat multidrug-resistant bacterial infections, so when bacteria develop resistance to them, treatment options can be extremely limited.
Laboratory Testing
To improve surveillance and awareness of CRE, the Florida Department of Health’s Bureau of Public Health Laboratories expanded CRE testing capabilities to identify types of resistance mechanisms used by organisms. Carbapenemase production is a resistance mechanism of concern. A carbapenemase is an enzyme that breaks down carbapenem antibiotics and can be transferred between organisms.
484 isolates tested for CRE mechanism in 2019
| Pseudomonas | 243 |
| Kiebsiella | 59 |
| Enterobacter | 37 |
| Escherichia | 27 |
| Candida | 21 |
| Serratia | 17 |
| Acinetobacter | 16 |
| Citrobacter | 7 |
| Other | 9 |
25% of isolates tested were carbapenemase-producing
| KPC | 70 |
| VIM | 26 |
| NDM | 36 |
| KPC and NDM | 8 |
| VIM and KPC | 2 |
| OXA-48-like | 2 |
A variety of carbapenemases have been reported in the U.S. and in Florida: Klebsiella pneumoniae carbapenemase (KPC), Verona integron-encoded metallo-beta-lactamase (NDM), and oxacillinase (OXA)-48-like. All laboratories participating in ELR must report antimicrobial resistance testing results for all Acinetobacter baumannii, Citrobater species, Enterococcus species, Enterobacter species, Escherichia coli, Klebsiella species, Pseudomonas aeruginosa, Serratia species, and S. aureus isolates from normally sterile sites. Resistance results are process electronically in the state’s reportable disease surveillance system.
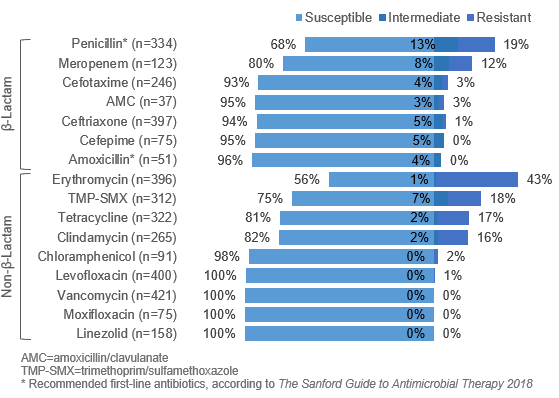
Streptococcus pneumoniae in 2019
- 760 S. pneumoniae invasive disease cases reported
- 40% had isolates resistant to at least one antibiotic
- 19% resistant to penicillin and 0% resistant to amoxicillin (recommended first-line antibiotics)
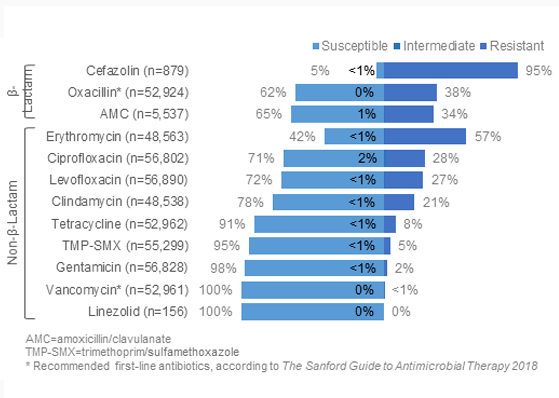
Staphylococcus aureus in 2019
- 58,368 isolates reported
- 38% resistant to oxacillin (i.e., MRSA) (susceptibility testing now done on oxacillin rather than methicillin)
- 0% resistant to vancomycin
(recommended first-line antibiotic when resistant to oxacillin)
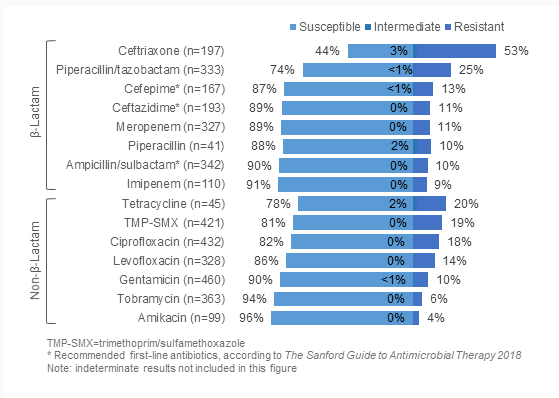
Acinetobacter species in 2019
- 511 isolates reported
- 11% resistant to one or more carbapenems (doripenem, ertapenem, imipenem, meropenem)
- 10%-13% resistant to recommended antibiotics: cefepime, ceftazidime, ampicillin/ sulbactam
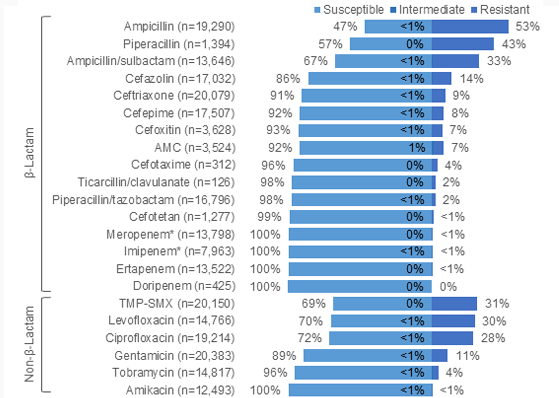
Escherichia coli in 2019
- 20,957 isolates reported
- 0.2% resistant to one or more carbapenems (i.e., CRE)
- <1% resistant to imipenem or meropenem
(recommended first-line antibiotics)
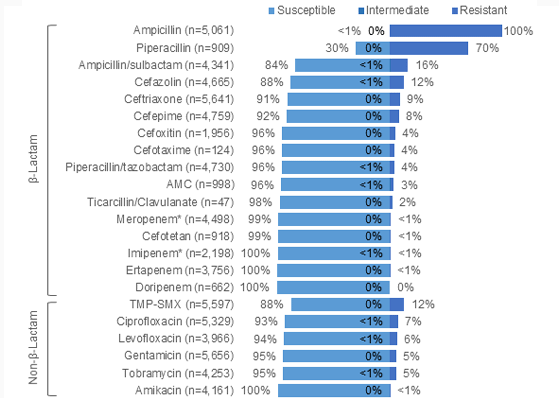
Klebsiella species in 2019
- 5,918 isolates reported
- 0.8% resistant to one or more carbapenems (i.e., CRE)
- <1% resistant to imipenem or meropenem
(recommended first-line antibiotics)
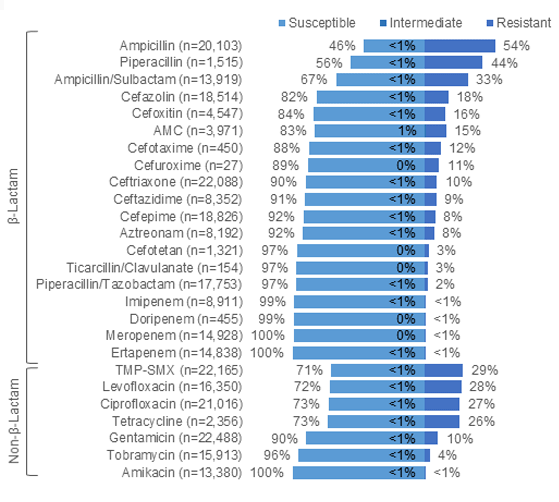
Enterobacteriaceae in 2019
- 28,166 isolates reported
- 0.6% resistant to carbapenem (i.e., CRE)
General Health Care-Associated Infection Resources
According to a recent federal survey, one in 25 hospital patients have a health care-associated infection (HAI).
The Agency for Healthcare Research and Quality has shown that the implementation of recommendations from the Healthcare Infection Control Practices Advisory Committee can reduce HAI by 70% overall and virtually eliminate some specific types of infections.
Strategic Plan: Prevent HAI and Antimicrobial Resistance
Developed by the Florida Department of Health’s Health Care-Associated Infection Prevention Program.
Multi-Drug Resistance Organisms (MDRO)
- Colonization Screening and Isolation Guidance
- Colonization Screening and Isolation Guidance in Acute Care Settings
- Guidelines for Prevention and Control
- Recommendations for Containment by Tier
Patients can also take action to help protect themselves from these types of infections:
- Speak up when receiving care and ask health care workers to wash their hands before touching you.
- If you are having surgery ask your doctor what you can do before surgery to help prevent infection or if you have a catheter, ask each day if it is still needed.
- Only take antibiotics when you need them, finish the course of treatment (do not stop taking your medicine when you begin to feel better), and remember that antibiotics typically are not effective against the common cold.
Isolation and Hygiene Signage
Prevention Resources
Florida Health Care-Associated Infection Program Information
Broad implementation of the guidelines saves lives, reduces suffering, and decreases health care costs. Through partnerships and the commitment of stakeholders, the Florida Department of Health’s Health Care-Associated Infection Prevention Program supports health care facilities implementing best practices for preventing the spread of HAIs.
Health care facilities are asked to conduct surveillance or track HAI infections, ensure health care workers perform hand hygiene before and after patient contact and when they come in contact with body fluids, use personal protective equipment such as gowns and gloves, minimize use of devices (e.g. catheters), and ensure the patient care environment has been cleaned including the proper cleaning of shared medical equipment, such as blood pressure cuffs and glucometers.
In addition, antibiotics need to be used wisely. Antibiotics do help fight infection, however overuse of antibiotics leads to the development and spread of multi-drug resistant organisms. Health care providers are asked to order cultures and review the results to ensure the most narrow spectrum antibiotic is used to treat infections.
Infection Control Training
The Health Care-Associated Infections Prevention Program of the Florida Department of Health has five separate web-based training modules on infection control, specifically created for facility nursing staff members in acute care hospitals, ambulatory care, and nursing homes. These trainings are available on-demand and at no charge. Each will satisfy one hour of continuing education units.
The training modules are available on the TRAIN Florida. If you do not have an account, you can create an account. You will be directed to a page that will ask for your professional license. You will need to choose your license and enter your license number to receive continuing education credit.
You can find the courses by searching for “FDOH Infection Control” and filtering the affiliate with “Florida.” You may select the class you want to take separately, or in a series by selecting the infection control series. With the series, you will take a brief Introduction course that will explain the course directions, the class “An Overview of Infection Control,” and select one course from the remaining classes dependent on your position and type of facility.
To register for the module
- Select the Registration tab, and then select Launch. Once completed, you will mark the course as completed. You will see a message stating Course was marked as “Completed.”
- You will need to take a 10-question quiz and post review.
- You need to score 70% on the quiz to pass the course, and you will need to post a review to receive credit for the class.
Blended Learning Series (Compilation)
Introduction and Overview (both classes are required)
- FDOH Infection Control Training: Introduction
- FDOH Infection Control Training: An Overview of Infection Control
Elective Modules (only one course from this section is required)
- FDOH Infection Control Training: Registered Nurses and Licensed Practical Nurses in Hospitals
- FDOH Infection Control Training: Registered Nurses and Licensed Practical Nurses in Nursing Homes
- FDOH Infection Control Training: Registered Nurses and Licensed Practical Nurses in Ambulatory Care
- FDOH Infection Control Training: Certified Nursing Assistants in Nursing Homes and Ambulatory Care
Each of these courses can be taken separately
- FDOH Infection Control Training: Introduction
- FDOH Infection Control Training: An Overview of Infection Control
- FDOH Infection Control Training: Registered Nurses and Licensed Practical Nurses in Hospitals
- FDOH Infection Control Training: Registered Nurses and Licensed Practical Nurses in Nursing Homes
- FDOH Infection Control Training: Registered Nurses and Licensed Practical Nurses in Ambulatory Care
- FDOH Infection Control Training: Certified Nursing Assistants in Nursing Homes and Ambulatory Care